UC developed a new biosensor that stimulates sweat on a tiny patch of skin. (Andrew Higley/UC Creative Services)
A better biosensor? No sweat
UC researchers develop an easy way to monitor biometrics with sweat, even when the patient is resting and comfortable.
By Michael Miller
513-556-6757
Aug. 3, 2017
One downside to medical sensors that test human sweat: You have to sweat.
Sweating from exertion or a stifling room temperature can be impractical for some patients and unsafe for others. And unless they are on the second leg of the Tour de France, it’s unlikely patients will want to sweat all day for the benefit of a sensor reading.
But researchers at the University of Cincinnati have come up with a novel way to stimulate sweat glands on a small, isolated patch of skin so subjects can stay cool and comfortable and go about their daily routine without spending hours on a treadmill.
UC professor Jason Heikenfeld and UC graduate Zachary Sonner came up with a device the size of a Band-Aid that uses a chemical stimulant to produce sweat, even when the patient is relaxed and cool. The sensors also can predict how much patients sweat, an important factor in understanding the hormones or chemicals the biosensors measure. The study was published July 25 in the nanotechnology journal Lab on a Chip.
“The challenge is not only coming up with new technological breakthroughs like this, but also bringing all these technology solutions together in a reliable and manufacturable device,” Heikenfeld said.
He co-founded a biosensor company, Eccrine Systems, Inc., that is pursuing just that.

UC professor Jason Heikenfeld works with firefighter Roger Rose to test sensors that can monitor the health of first responders in this 2013 file photo. (Dottie Stover/UC Creative Services)
Biomedical sensors are part of a medical-device industry valued at $88 billion in the United States, according to the market-research firm IbisWorld. The industry is poised to see explosive growth in the next five years with the advent of new technology and increasing competition.
Heikenfeld helped launch the Cincinnati biosensor company in 2013 with help from UC’s Technology Accelerator program. He serves as Eccrine System’s chief science officer and was recently named UC’s assistant vice president of entrepreneurial affairs and technology commercialization.
The company’s work is attracting international attention because of the profound way that it could change health diagnosis and monitoring, he said.
"Doctors would love to know if chemical concentrations are increasing or decreasing over time," Heikenfeld said. "What was your baseline before you got sick? Then by measuring the change in concentrations, we know even more about how sick you are or how quickly you are getting better."
Blood analysis is considered the gold standard for biometric analysis. But biometric testing with blood is invasive and often requires the use of a lab. It is far more difficult for doctors to perform continuous monitoring of blood over hours or days.
Sweat provides a noninvasive alternative, with chemical markers that are more useful in monitoring health than saliva or tears, Heikenfeld said.
“People for a long time ignored sweat because, although it can be a higher-quality fluid for biomarkers, you can’t rely on having access to it,” Heikenfeld said. “Our goal was to achieve methods to stimulate sweat whenever needed — or for days.”
“Imagine being able to monitor cardiac patients after they have been released from the hospital, or preventing dehydration in athletes or even helping ensure that your body is getting the exact right concentrations of a prescription drug.”
‒ Jason Heikenfeld, director of UC's Novel Devices Laboratory
Heikenfeld, also director of UC’s Novel Devices Laboratory, has been studying the problem for seven years. Scientists say sweat provides much of the same useful information about patients as blood. The problem has always been getting the same consistent sample as is possible with a standard blood draw, he said.
“We believe that the solutes you find in blood you will find in sweat,” he said. “We have postulated that for some time and, as of right now, have not seen anything to change our hypothesis.”
Testing sweat has other possible benefits over blood, he said.
“If you do a blood draw, you get one data point,” he said. “In many cases, doctors would love to know if concentrations are increasing or decreasing over time.”
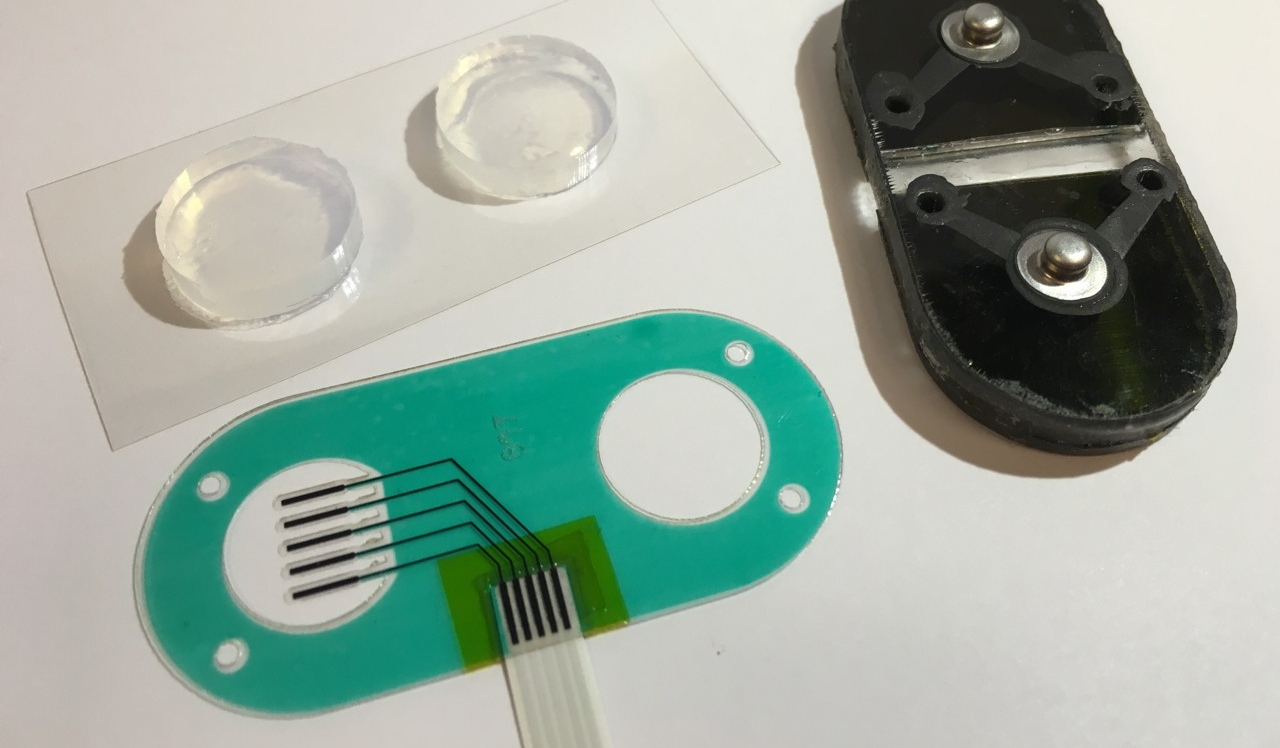
The UC study used a low electric current and carbachol gel to stimulate sweat under a sensor the size of a Band-Aid. (Photo provided)
For the study, the researchers applied sensors and a gel containing carbachol, a chemical used in eyedrops, to their subject’s forearm for 2.5 minutes.
They used three methods to obtain sensor data: the gel and sensors alone and in combination with memory foam padding (to provide better contact between the sensor and the skin) and iontophoresis, an electrical current at 0.2 milliamps that drives a tiny amount of carbachol into the upper layer of the skin and locally stimulates sweat glands but causes no physical sensation or discomfort.
Then they recorded data obtained from the subject’s sweat for 30 minutes using sensors that measured concentrations of sweat electrolytes. Carbachol was effective at inducing sweating under the sensor for as long as five hours. Heikenfeld said a subsequent study successful generated sensor results for several days using this process to stimulate sweat.
They used a pH-sensitive dye to observe the results. The orange dye turned blue when it reacted with sweat. This demonstrated that the sweat glands were stimulated evenly across the sensor area.
“This work represents a significant leap forward in sweat-sensing technology,” the study concluded.
“Imagine being able to monitor cardiac patients after they have been released from the hospital, or preventing dehydration in athletes or even helping ensure that your body is getting the exact right concentrations of a prescription drug,” Heikenfeld said.
“The ultimate goal is convenience and reliability for biomedical applications,” said alum Sonner, lead author of the paper.
“The end goal is to take the idea from a benchtop test to a portable device — perhaps for people in high-stress jobs like airline pilots — and analyze them for stress,” Sonner said. “If you’re a pilot, you can’t do blood draws while you’re flying the plane. But a sensor could analyze sweat so we can begin to understand how their body responds to stressful situations.”
The study comes at a time when many consumers are taking a more active role in monitoring their own body chemistry and using wearable technology to track their progress toward some athletic or wellness goal.
The sensors UC developed could help track changes in hormones such as cortisol, which is released when someone is under stress.
“Cortisol levels can help trainers know just how hard they need to train an athlete until they are pushing them too far,” he said.
That is the moment when athletic performance begins to drop off while the chance of injury dramatically increases, he said.
Possible uses go well beyond Olympic athletes. The U.S. Air Force Research Laboratory at Wright-Patterson Air Force Base, a UC research partner, is extremely interested in measuring cortisol in pilots facing mentally and physically stressful situations. Monitoring their health and performance over time using noninvasive sensors would be extremely helpful, Heikenfeld said.
Likewise, it could be useful for patients who might want to perform regular health monitoring at home after a surgery, Sonner said.
“It’s particularly useful for follow-up visits where normally there is some type of blood testing that has to be done. They could wear a disposable patch for 20 minutes instead,” Sonner said.
And saving the time and money of an unnecessary trip to the blood lab or doctor’s office: totally worth the sweat.

UC engineering professor Jason Heikenfeld. (Lisa Ventre/UC Creative Services)
Better living through engineering
Do you like to work on research? At UC, students at the College of Engineering and Applied Science tackle real-world problems that improve people's lives. Explore programs on the undergraduate or graduate level.

